LARS (LOW ANTERIOR RESECTION SYNDROME) is a condition that can affect individuals after undergoing bowel surgery, particularly for rectal cancer. Many patients have questions about what to expect, how symptoms may change over time, and what treatments or lifestyle adjustments can help. In this section, we address some of the most frequently asked questions about LARS to help patients and their caregivers better understand and manage the condition.
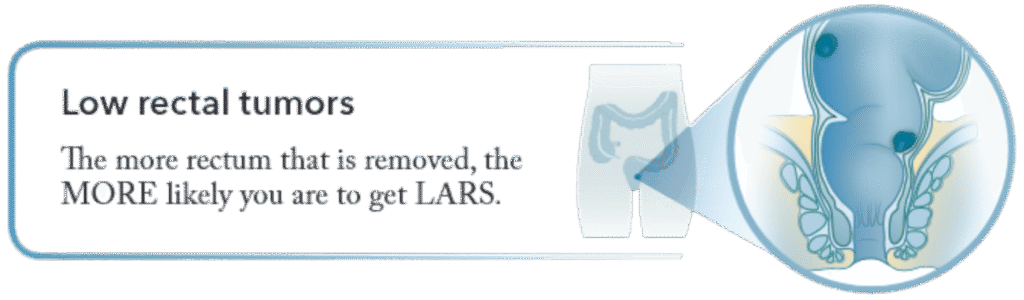
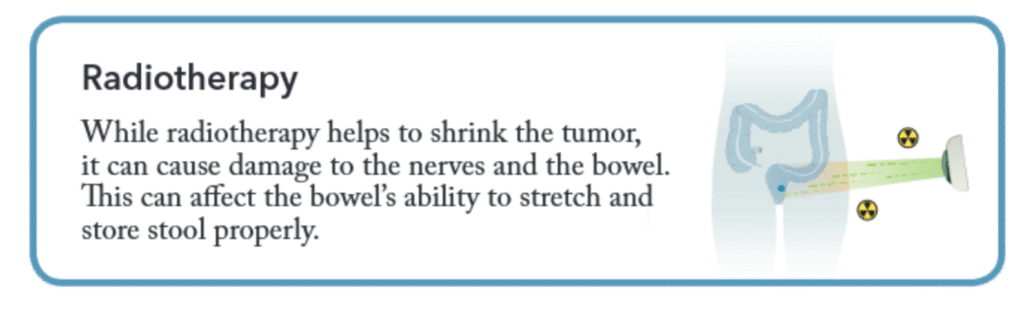
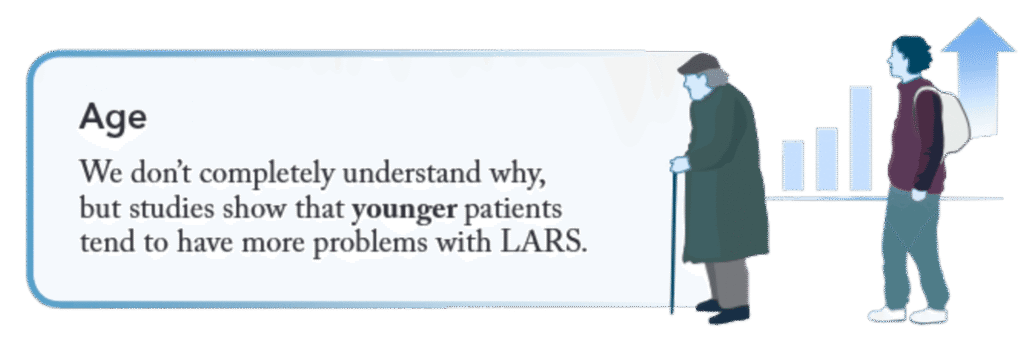
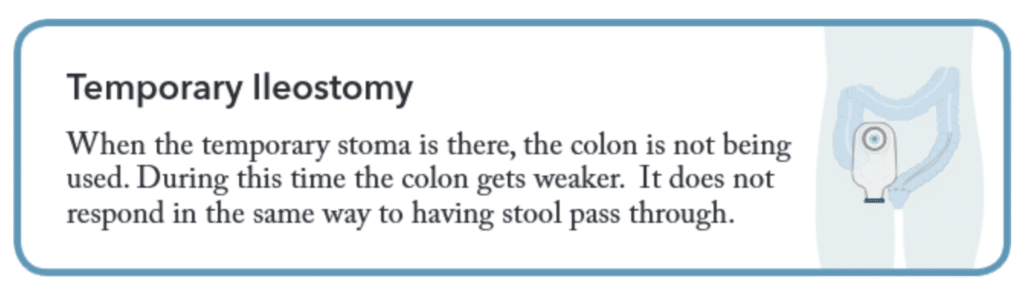
There is no single cause for LARS. For most patients,
it is probably a combination of things. Here we list
some of the common causes that we think about, but
others may exist too.
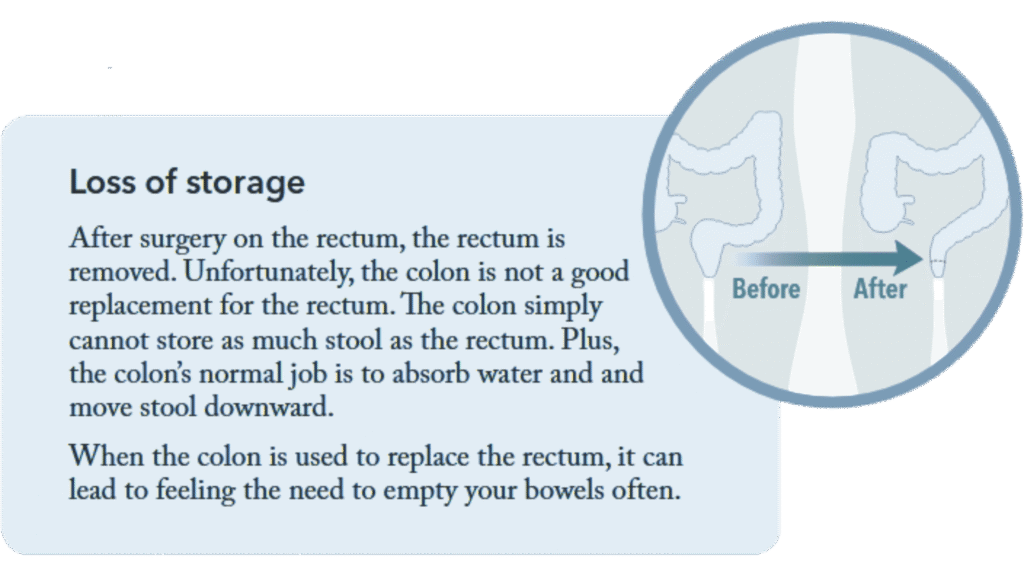
Here are some of the main factors:
How common is LARS?
How is LARS diagnosed?
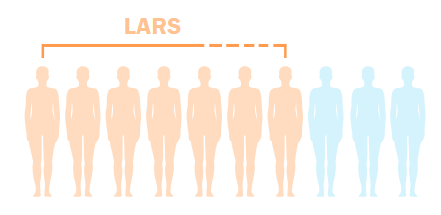
LARS seems to affect 5 to 7 out of every 10 patients after Low Anterior Resection
surgery, with more than half of patients saying that it affects their quality of life.
Even people who DON’T have rectal cancer surgery can have these types of
symptoms (e.g. accidental leakage, frequent bowel movements). So you are definitely
not alone if you experience LARS.
Unlike other medical problems, LARS is not diagnosed with
blood tests, x-rays, or biopsies. The diagnosis of LARS is
based on your symptoms.
We normally say that you have LARS if your bowel
symptoms have lasted more than 1 month since your
Low Anterior Resection surgery (or the removal of your
temporary stoma).
For most patients, LARS symptoms are usually worse
immediately after surgery, and improve slowly during
the first 2 years after surgery. It is hard to know for
sure what your experience will be, if your symptoms
will improve, and how long they might last.
Even if LARS might be long term, generally, you can
expect to reach a new baseline after about 2 years.
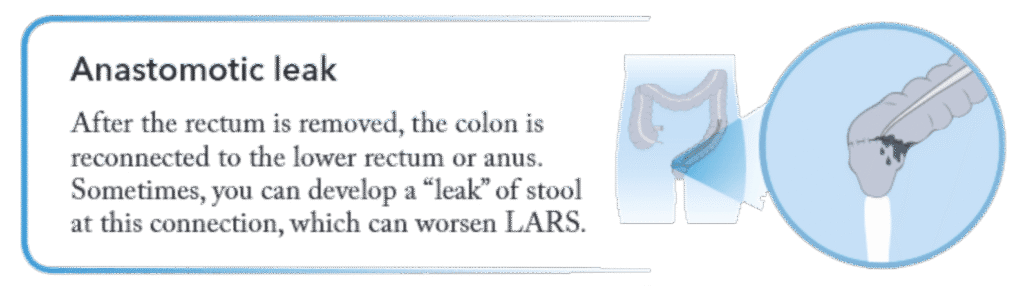
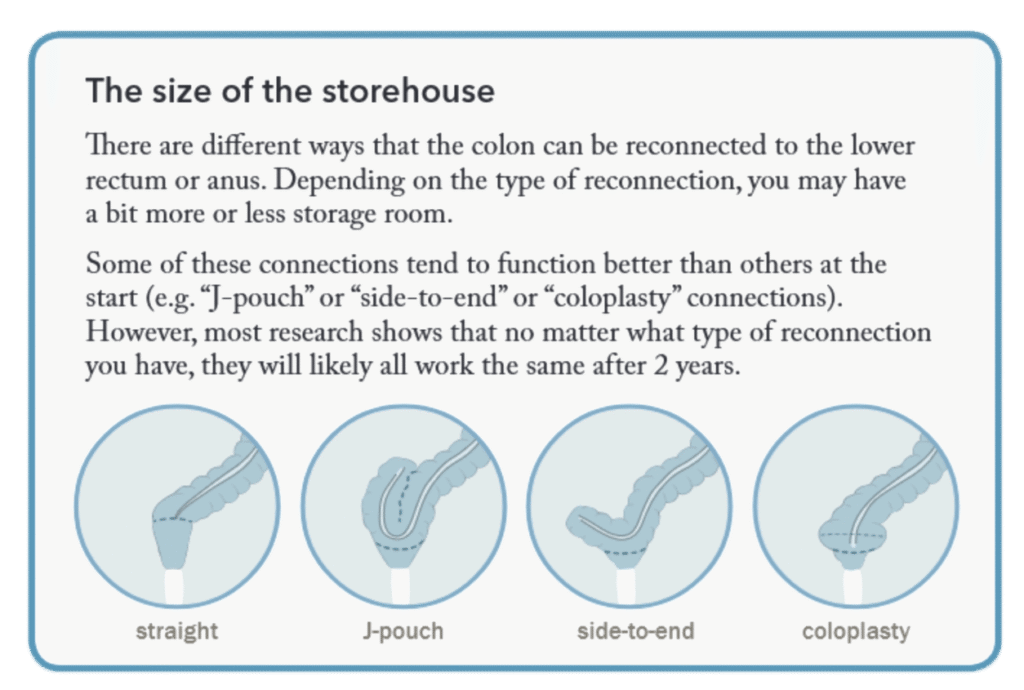
It could also be that your bowels (the
colon from above that is reconnected to
the lower rectum or anus) adapts over
time to be able to accommodate more
stool and act as a better storehouse.
In addition, patients learn to live with
their LARS and find strategies to deal
with their “new normal”.